LOC While Breath-Hold Diving
Diving Medicine
By Dr. David Sawatzky
In this column we will look at the breath-hold diver who suddenly looses consciousness in relatively shallow water. These individuals often die from drowning. This phenomenon has been called ‘shallow water blackout’ but the term should be avoided – it’s confusing. Initially shallow water blackout was used to describe divers who had passed out from too much carbon dioxide while diving on a rebreather. It was subsequently used to describe breath-hold divers who passed out from too little oxygen. Therefore, we will simply call it ‘loss of consciousness’ (LOC) while breath-hold diving. There are two situations where this relatively common problem occurs.
Breathing has both voluntary and involuntary control. What this means is that we can control our breathing consciously. We can hold our breath, we can breathe rapidly and deeply or slowly and shallow, etc., all within certain limits. But, if we stop thinking about breathing it happens automatically. This is very important; otherwise we would stop breathing every time we fell asleep!
The respiratory control center in the brain regulates our breathing. It sends a signal to the diaphragm causing it to contract. The diaphragm is a large flat muscle that stretches across the body, separating the chest from the abdomen. When it is relaxed, it rises up into the chest cavity like the top half of a balloon; when it contracts, it flattens and descends into the abdomen. This causes the volume of the chest cavity to increase. The lungs are sponge like structures held against the chest walls by suction. As the volume of the chest cavity increases, the lungs expand to fill the space, pulling air in through the mouth/nose.
During quiet breathing, at the end of inspiration the diaphragm relaxes. The elastic fibers in the lungs were stretched during inhalation so when the diaphragm relaxes, the elastic fibers cause the lungs to contract. This pushes air out of the lungs. As the lungs contract the diaphragm is pulled back up into the chest cavity. Therefore, during quiet respiration inhalation is an active process resulting from contraction of the diaphragm while expiration is passive and results from the elastic recoil of the lungs and other tissues.
When we exercise we need to move more air in and out of the lungs. We accomplish this by taking deeper breaths. As the diaphragm contracts the chest wall muscles also contract, pulling the ribs up and out. The ribs attach at the front and back and can be thought of as bucket handles hanging down on each side of the chest. As they are pulled up, the chest expands laterally and the chest cavity volume is further increased.
We can also increase respiration by exhaling more fully. We accomplish this by contracting our abdominal wall muscles to push the diaphragm up into the chest and by contracting chest wall muscles to pull the ribs further down. Both of these actions result in a decrease in the chest cavity volume, forcing more air out of the lungs.
As a result of the involvement of these other muscles, we can move much more air in and out of our lungs with each breath and we can breathe more rapidly. Under these circumstances both inspiration and expiration are active processes.
The primary purpose of breathing is to move oxygen (O2) into the lungs/body and to move carbon dioxide (CO2) out. The respiratory control center in the brain monitors the levels of O2 and CO2 in the blood and controls the rate and depth of breathing to maintain these molecules at a constant level (partial pressure). Surprisingly, the respiratory control center responds weakly to the levels of O2 in the blood. This means that abnormally high or low levels of O2 in the blood have a limited effect on the rate and depth of breathing. The respiratory control center responds primarily to the level of CO2 in the blood.
A simple example will help clarify this. We do not increase respiration until we have been exercising for a minute or two and we continue to breathe heavily for several minutes after we have stopped. This makes perfect sense. When we commence exercise the level of CO2 in our blood is normal. As our muscles perform work they use up their supply of ATP. O2 is used to generate more molecules of ATP, and CO2 is produced as a waste product. The CO2 diffuses out of the muscles into the blood and is carried back to the heart and eventually up to the head where the respiratory control center senses it. It takes a minute or two for the levels of CO2 in our blood to rise when we start exercising and therefore it is a minute or two after we start exercising before the respiratory control center senses the rising CO2 and sends signals to increase the depth and rate of breathing.
When we stop exercising the muscles continue to use O2 and generate CO2 for several minutes to replenish the ATP used during exercise. Therefore, we continue to breathe heavily for a few minutes after we stop exercising.
When we hold our breath the level of CO2 in the blood starts to rise (normal is around 40 mmHg). As the level of CO2 rises, the respiratory control center sends increasingly strong signals to the diaphragm and other muscles involved in breathing to try and move more air in and out of the lungs to lower the level of CO2. We can consciously override this signal for a limited period of time before we are forced to start breathing again (normally around a CO2 level of 50 mmHg).
The level of CO2 in the blood rises when we are holding our breath because O2 is being used to generate energy. Therefore, as the level of CO2 rises, the level of O2 is falling (normal is around 100 mm Hg). Our bodies are very well designed and we can tolerate a significant fall in the level of O2 without any difficulties. The net effect is that a person holding their breath while relaxing will be forced to start breathing due to the rising level of CO2 before the falling level of O2 becomes a problem, assuming that they did not hyperventilate before they held their breath.
Hyperventilation is consciously breathing faster and deeper than is required to maintain a normal level of CO2 in the blood. The result of hyperventilation is that too much CO2 is removed from the blood and the level of CO2 in the blood will be reduced (often to 30 mmHg). If the level of CO2 is reduced too much the person will start to notice tingling around their mouth, tingling of their hands and feet and other symptoms. However, a limited amount of hyperventilation will cause no symptoms.
If a person hyperventilates and then holds their breath, it will take much longer for the CO2 in the blood to rise to the level where they are forced to breath (they will be able to hold their breath longer). The problem is that if you hold your breath longer, the partial pressure of O2 in the blood can be reduced to a level where symptoms occur. The first symptom of hypoxia (too low a level of O2 in the blood) is often loss of consciousness.
Several thousand people die every year in North America from drowning. In those cases where a person survives a LOC while breath-hold diving, virtually every one had hyperventilated before holding their breath. In most cases they had also been working. Again, this makes perfect sense. If you are working while holding your breath, the level of O2 in the blood will drop faster making it more likely that you will loose consciousness.
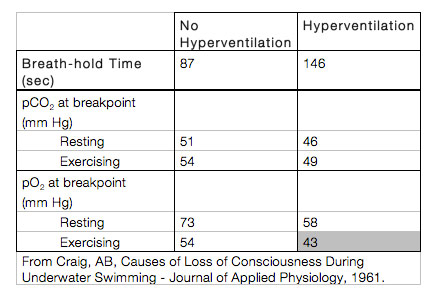
There have been many studies performed to document these events but the one from 1961 shown in the table demonstrates this very nicely. Hyperventilation clearly increases breath-hold time but, when combined with exercise, results in a level of hypoxia that often causes loss of consciousness.
The bottom line for breath-hold diving is that you should not hyperventilate before doing a breath-hold dive.
The second way in which you can loss consciousness while breath-hold diving is if you dive deep (after hyperventilating). While you are at depth you have lots of O2. The increased pressure at depth increases the partial pressure of O2 in the blood. However, when you ascend the pO2 in the blood drops rapidly and the diver often looses consciousness just before surfacing. In competitions where breath-hold divers are attempting to see how deep they can go, safety divers are positioned along the ascent line to deal with this relatively common event.
Divers lose consciousness as a result of hypoxia while breath-hold diving in two common situations. The physiology of this problem is well understood, as explained. The problem can be avoided by simply not hyperventilating before a breath-hold dive.
This problem can also be avoided by hyperventilating on 100 percent O2 before a breath-hold dive. Unfortunately, if you breathe 100 percent O2 and then dive deeper than 10 feet of seawater (3msw), pO2 = 1.3 ata, you risk loss of consciousness from oxygen toxicity.
One Response to “LOC While Breath-Hold Diving”
Leave a Comment




Moe
Great article Dr. Sawatzky. I have a question however; when you talk about breath holding dives, do you mean divers who take a breath, attempt to hold it a bit then let it out slowly (to conserve oxygen)? Or are you referring to divers who basically attempt to hold breath underwater to see how long they can last without needing another?
And for that matter, what do you suggest to divers who’d like perfect their underwater breathing to maximize their bottom time and avoid being labeled as “air suckers”?