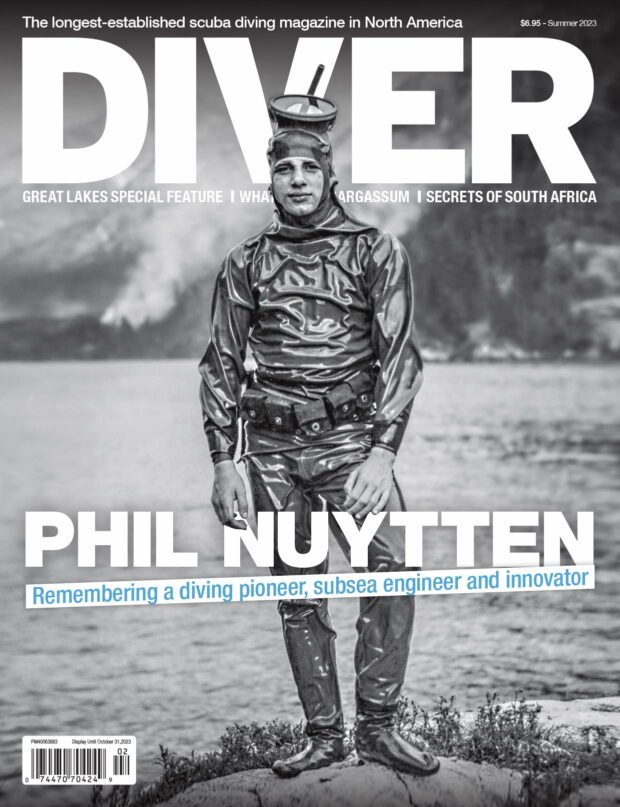
BPPV – Sudden onset of vertigo

By Dr. David Sawatzky
Recently I’ve been exchanging emails with a diving friend who experienced sudden, severe, nausea, vomiting and vertigo after a dive in Mexico. DAN diagnosed inner ear barotrauma and the local Ears, Nose and Throat (ENT) specialist diagnosed Benign Paroxysmal Positional Vertigo (BPPV). Upon return to Canada he underwent several investigations and so far the working diagnosis is BPPV, although his symptoms don’t fit the definition of BPPV very well.
In DIVER June 2009, I wrote about Inner Ear Barotrauma, in the July/August issue I covered Balance and Disorientation and in the September issue I reviewed Inner Ear Decompression Sickness. Divers need to know about these serious problems that can be caused by diving but they should also know about the most common cause of vertigo, which is BPPV.
‘Vertigo’ is often confused with ‘dizziness’. In vertigo, the world is ‘spinning’. Basically what’s happening is that one or both of your inner ears are telling your brain that your head is moving. The brain sends a signal to the muscles that control movement of the eyes and moves them exactly opposite the movement of the head.
When the system is working properly, this allows us to see clearly when our heads are moving. If we did not have this ability, everything would be blurry when we moved our heads.
As a quick example, look at the text you are reading and move your head back and forth. It is easy to continue reading the text because as your head moves, your eyes move to continue looking in the same direction.
What happens in vertigo is that the inner ears tell the brain that the head is moving when in fact it is not. The brain moves the eyes to compensate for the movement of the head, except the head is not moving. As a result whatever the person is looking at seems to move (i.e. the world spins).
Balance and Disorientation
Basically, the inner ear has two structures that are involved in balance and orientation.
The semicircular canals are oriented perpendicular to each other so that one is in each of the X, Y, and Z planes. Imagine three circles on the surfaces of a cube, one on the bottom and the other two on the sides, all joined at one corner. These canals are filled with fluid. As the head moves, the fluid will lag behind the movement of the head due to inertia. This will cause the fluid to move in the canals.
Each canal contains an area where hairs project into the fluid. As the fluid moves, the hairs are moved and signals are sent to the brain. The brain integrates the signals from all the canals, calculates exactly how the head has moved, and sends signals to the muscles that control the eyes to move them exactly opposite the movement of the head.
When the head stops moving, the fluid will continue to move for a short time, moving the hair cells in the opposite direction.
It is relatively easy to make the system generate incorrect information. Try the following but only when someone else is around to prevent you from falling and hurting yourself. Sit in a chair or on a stool that can rotate. Rotate the chair at a constant speed for about 15 seconds (keep your eyes closed). Then suddenly stop the chair/stool and open your eyes.
You will see the world moving sideways for several seconds before it stops, and most people will feel quite nauseated. What has happened is that the fluid initially lagged behind the movement of the head when you started to rotate but over the 15 seconds or so it caught up so that it was moving as the same speed as your head. When you stopped suddenly the fluid continued to move for several seconds until it slowed down and stopped. Your brain integrated the signals from your inner ears and moved your eyes to compensate for the “assumed” movement of your head (your head was not moving). As a result, you saw the world seem to move sideways. If someone else looked at your eyes while the world appeared to be spinning, they would see your eyes moving sideways (nystagmus).
We have other sensors in our bodies that were telling our brains that, in fact, the world was not moving sideways and that the contradictory information generated the feeling of nausea. If this stimulus is strong enough, you will vomit.
The inner ears also contain a different kind of sensor in the Utricle and Saccule. These sensors are also hair cells but the hairs have a ‘crystal’ or ‘ball of calcium’ hanging from the end. Gravity pulls on these crystals and the hair cells send signals to the brain to tell it how the head is located relative to the pull of gravity. Even with your eyes closed you know which way is ‘down’.
BPPV Most Common
There are a very large number of causes of vertigo but the most common is Benign Paroxysmal Positional Vertigo (BPPV). BPPV is when a person experiences sudden onset of vertigo that usually lasts only a few minutes and then goes away. The vertigo may be mild, moderate or very intense.
These episodes of vertigo are not caused by an illness (benign), they tend to occur frequently (paroxysmal), and the symptoms are often caused by a change in the position of the head (positional).
In cases of BPPV, some of the crystals that are normally attached to the hair cells in the Utricle and Saccule break off and move freely in the fluid. If they move into the semicircular canals they can stimulate the hair cells there sending signals to the brain that the head is moving when it’s not.
There are several reasons that crystals can become detached from the hair cells in the Utricle and Saccule. The most common is a blow to the head, even a relatively mild blow, or a sudden movement of the head. Repetitive movements of the head (working at a computer, dusting or cleaning above your head), viral infections, inflammation, and ear surgery can also cause BPPV.
Other than the potential causes mentioned above, the only real risk factor for BPPV is age. BPPV can occur at any age but is most common in those over age 60.
Other than vertigo, the signs and symptoms of BPPV usually include nausea and may include vomiting, lightheadedness, loss of balance, unsteadiness and/or blurred vision.
The diagnosis of BPPV is usually based on the inability to find any other problem to explain the vertigo and the ability to reproduce the vertigo with specific head movements. If the history is clear enough no investigations may be required. If the history or examination has unusual findings, investigation may be required to identity or rule out other causes of vertigo. Ear, nose and throat (ENT) specialists and/or neurologists may need to be involved in making the diagnosis.
BPPV is treated in several ways. The most common is a specific series of head movements that attempt to move the crystals from the semicircular canals back into the vestibule where they will not cause symptoms and may be reabsorbed. The movements required depend on which semicircular canal the crystals are in. These movements may have to be repeated.
Other movements may be prescribed whose purpose is to accelerate habituation of the brain to the altered signals with the resultant resolution of the symptoms.
Common sense precautions such as not being in a place where sudden vertigo could be dangerous, sitting down immediately when the vertigo starts and waiting for it to pass, and avoiding head movements that trigger the vertigo will help. BPPV usually resolves over time but may recur. In severe cases where treatment is not effective, the involved semicircular canal can be surgically blocked. This surgery is 90 per cent effective in controlling the symptoms but it destroys the function of that semicircular canal.
Drugs can be used to help control the symptoms (antihistamines, anticholinergics, sedative/hypnotics) but they are often not very effective.
BPPV is common, especially in older individuals. Many divers will develop this problem and the onset may be after a dive. The condition is usually not severe and can usually be treated effectively.
Many other causes of vertigo exist and in divers it is important to identity inner ear barotrauma and inner ear decompression sickness. Fortunately, BPPV is far more common than either inner ear barotrauma or inner ear DCS.
7 Responses to “BPPV – Sudden onset of vertigo”
Leave a Comment




margo parenti
i am going on 63 and have positional vertigo. I am planning on getting certified for diving. I wonder if this is a good idea or not.
Richie
Glad I found this article, I have been diagnosed with BPPV and ETD ???? my final dive ended badly when I began to get extremely nauseated during the dive, I ascended and upon breaking the surface all hell let loose, it was akin to being horribly drunk ! Resulting in vomiting and feeling poorly for about 24 hours after (residual effects of motion sickness)
Dive instructor was a bit worried referring to his tables etc (in fear I had bent myself) however I was confident that it was not an issue with the dive profile, but rather an issue with me !
Some tips if I may ?
1) upon becoming nauseated, I found looking down at the sea floor made matters worse, the flickering of light from the waves above added to my brains confusion !
2) STOP ! Position yourself vertical and focus on a static object in the distance, give your brain a chance to catch up
3) slow ascent !! Changes in pressure can set off vertigo (altonobaric) I found ascending in stages and gradually helps
Spend some time floating on the surface before you have to stand bearing your own full weight (this also triggered the vertigo)
4) stay calm and don’t panic…. Don’t rush yourself to the pot of its not going to do you any good ????
Hope this helps some folk, it has alas ended my diving for me, for which I am devastated !
Faythe
guess I am in good company. I knew I had recent history of BPPV and long long history of motion sickness…and migraines. Had always managed the motion sickness while diving by getting in water quickly, not getting overheated. But my first dive in 16 years ended in disaster. Got horribly sick on surfacing in chop. Since then I’ve been preoccupied with how to manage the motion sickness [shore vs. boat]. But I realize if I can get vertigo from rolling over in bed, I could get it deep under water. And I just spend $2k on dive equipment. waaah.
Jeff Bailey
Sounds like your dive instructor was dangerously ignorant of post diving illnesses if he was worriedly looking at dive tables and did anything other than the following. Any serious or neurological symptoms within 10 minutes of surfacing and especially immediately upon surfacing should have been followed by an immediate on site neurological assessment and immediate administration of O² and transport to nearest recompression chamber.
Luckily, your issue was not a lung overexpansion issue or arterial gas embolism (AGE), which can lead very quickly to paralysis or death. AGE can happen regardless of dive profile (yes, even with a 1 minute dive to 10′), and the associated symptoms do not even indicate looking at the dive profile. Luckily, your condition turned out not to be caused by this. But the aforementioned protocol still should have been followed.
Kat
I have been diagnosed with bppv. Ended my diving career as well. Even snorkeling is a challenge – I get nauseous if I’m upright. Only works when I’m snorkeling laterally. People who don’t know what bppv is will say no just go slow you. An get through this but unless you enjoy feeling horrible and vomiting into your mouthpiece then I’d advise against it. Sorry. It sucks.
jack gregory
I experienced the same thing as others..BPPV.. after my third dive of the day, it hit! Fortunately my daughter was with me and had experienced BPPV a few years ago and knew the exercises. It still took me 3 days of doing nothing but laying on the couch and sleeping as walking was impossible. Symptoms have mostly disappeared after a week. The diving was great, the BPPV was a rotten 70th birthday present as I missed a great night dive!
Sally
I’d be interested to hear from people who have had BPPV, been successfully treated using the Eply manoeuvre and been able to return to diving (or not!). I had BPPV earlier this year for a few weeks and the Eply manoeuvre completely sorted it out for me.
I’ve been fine since but am a little nervous about heading off on a liveaboard in case it comes back. I’m thinking I may stick to shore diving for my next trip, just in case.
Does anyone else have experience of this?